When Samantha Deffler was young, her mother would often call her by her siblings’ names — even the dog’s name. “Rebecca, Jesse, Molly, Tucker, Samantha,” she says.
A lot of people mix up children’s names or friends’ names, but Deffler is a cognitive scientist at Rollins College, in Winter Park, Fla., and she wanted to find out why it happens. So she did a survey of 1,700 men and women of different ages, and she found that naming mistakes are very common. Most everyone sometimes mixes up the names of family and friends. Her findings were published in the journal Memory & Cognition.
“It’s a normal cognitive glitch,” Deffler says.
It’s not related to a bad memory or to aging, but rather to how the brain categorizes names. It’s like having special folders for family names and friends names stored in the brain. When people used the wrong name, overwhelmingly the name that was used was in the same category, Deffler says. It was in the same folder.
And there was one group who was especially prone to the naming mix-ups.
“Moms, especially moms,” Deffler says. “Any mom I talked to says, ‘You know, I’ve definitely done this.'”
It works something like this: Say you’ve got an armful of groceries and you need some quick help from one of your kids. Your brain tries to rapidly retrieve the name from the family folder, but it may end up retrieving a related name instead, says Neil Mulligan, a cognitive scientist at UNC Chapel Hill.
“As you are preparing to produce the utterance, you’re activating not just their name, but competing names,” he says. You flick through the names of all your other children, stored in the family folder, and sometimes these competing names win.
Like in the classic scene from the TV show, Friends. When Ross says his wedding vows, he is asked to repeat his fiancée’s name, Emily. He says his former girlfriend’s name Rachel instead.
Now Ross probably had both Rachel’s and Emily’s names in his mental folder of loved ones and a mental mix-up ensued.
And it’s not just human loved ones that are filed together.
“Whatever dog we had at the time would be included in the string along with my sister Rebecca and my brother Jesse,” Deffler says.
So your family dog typically gets filed with other family members. This of course sparks the question — what about your family cat?
“You are much more likely to be called the dog’s name than you are to be called the cat’s name.” Deffler says.
This implies that psychologically, we categorize the dog’s name along with our family member’s names, according to Mulligan.
“And we don’t do that with cats’ names, apparently, or hamsters’ names or other animal names,” Mulligan says.
Maybe that’s why we call the dog man’s best friend.
Source: NPR
Today our Director of Operations, Jenna Schrumpf, is in Lansing to meet with fellow brain injury advocates and legislative leaders. We invite you to follow along her day in our Capitol Day interactive timeline!
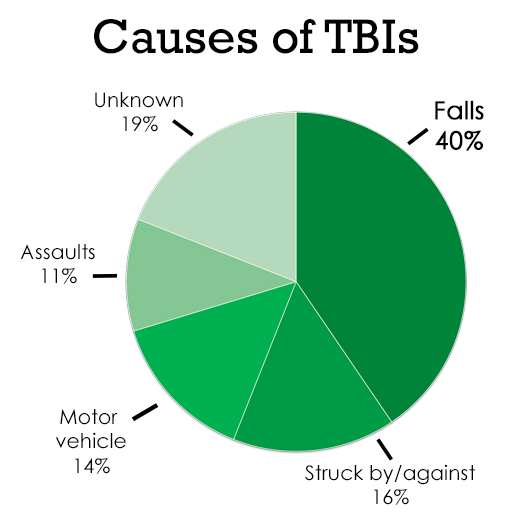
According to the Brain Injury Association of America (BIA), “…every day, 137 people in the U.S. die because of a TBI-related injury…” (BIA, 2015). So, what is the leading cause of these Traumatic Brain Injuries? It may not be what you think.
When you hear someone has suffered or survived a Traumatic Brain Injury (TBI), does the scene of a car accident flash through your head? At only 14.5%, motor vehicles are actually the 3rd leading cause of TBIs.
The number one cause of many TBIs is due to falls.¹
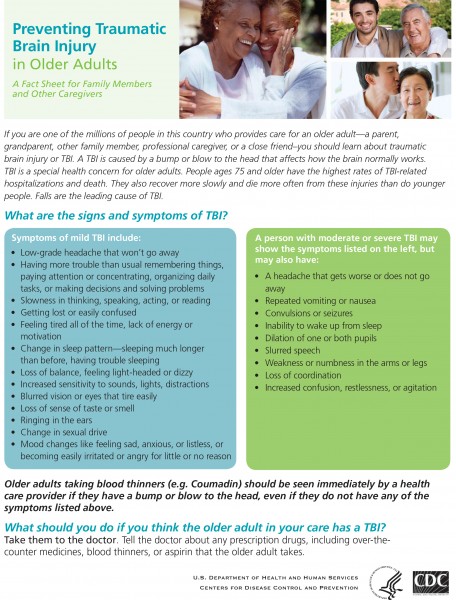
It is also no coincidence that Brain Injury Awareness Day (March 16) is in the middle of National Patient Safety Week (March 13-19). As a healthcare provider, it is important that we pass along information to protect our clients and our families. Below is a compiled list of fall risk factors as well as prevention and safety tips.
What Conditions Make You More Likely to Fall?²
Research has identified many conditions that contribute to falling. These are called risk factors. Many risk factors can be changed or modified to help prevent falls. Please note that most falls are caused by a combination of risk factors. The more risk factors a person has, the greater their chances of falling. They include:
- Lower body weakness
- Vitamin D deficiency (that is, not enough vitamin D in your system)
- Difficulties with walking and balance
- Use of medicines, such as tranquilizers, sedatives, or antidepressants. Even some over-the-counter medicines can affect balance and how steady you are on your feet.
- Vision problems
- Foot pain or poor footwear
- Home hazards or dangers such as
- Broken or uneven steps,
- Throw rugs or clutter that can be tripped over, and
- No handrails along stairs or in the bathroom.
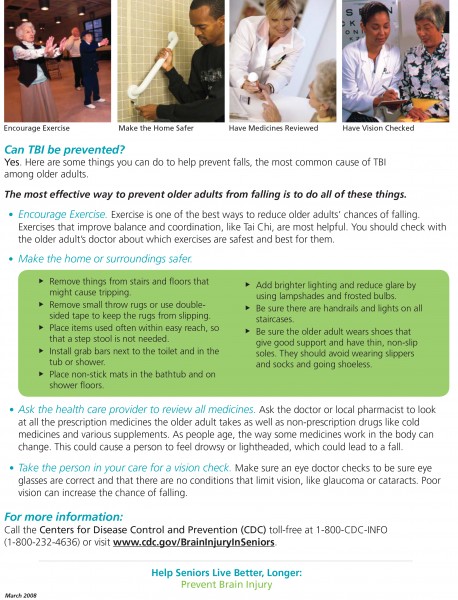
Prevention Tips³
You can play a role in preventing falls. Encourage the older adults in your life to:
- Get some exercise. Lack of exercise can lead to weak legs and this increases the chances of falling. Exercise programs such as Tai Chi can increase strength and improve balance, making falls much less likely.
- Be mindful of medications. Some medicines—or combinations of medicines—can have side effects such as dizziness or drowsiness. This can make falling more likely. Having a doctor or pharmacist review all medications can help reduce the chance of risky side effects and drug interactions.
- Keep their vision sharp. Poor vision can make it harder to get around safely. Older adults should have their eyes checked every year and wear glasses or contact lenses with the right prescription strength to ensure they are seeing clearly.
- Eliminate hazards at home. About half of all falls happen at home. A home safety check can help identify potential fall hazards that need to be removed or changed, such as tripping hazards, clutter, and poor lighting.
Steps for Home Safety³
The following checklist can help older adults reduce their risk of falling at home:
- Remove things you can trip over (such as papers, books, clothes, and shoes) from stairs and places where you walk.
- Install handrails and lights on all staircases.
- Remove small throw rugs or use double-sided tape to keep the rugs from slipping.
- Keep items you use often in cabinets you can reach easily without using a step stool.
- Put grab bars inside and next to the tub or shower and next to your toilet.
- Use non-slip mats in the bathtub and on shower floors.
- Improve the lighting in your home. As you get older, you need brighter lights to see well. Hang lightweight curtains or shades to reduce glare.
- Wear shoes both inside and outside the house. Avoid going barefoot or wearing slippers.
More Information
For more information about Fall Prevention, download these Stopping Elderly Accidents, Deaths, & Injuries (STEADI) safety brochures: what_you_can_do_brochure-a; check_for_safety_brochure-a.
To learn more about Traumatic Brain Injuries, visit the Brain Injury Association of Michigan. For more statistics about TBIs, download this Centers for Disease Control and Prevention flyer: Brain Injury Statistics.
If you or a loved one are a TBI survivor and need assistance in your home, give us a call at
866-866-8984!
¹BIA. (2015). Brain Injury Fact Sheet. Retrieved March 15, 2016.
²CDC. (2015, September 21). Important Facts about Falls. Retrieved March 15, 2016.
CDC. (2015, September 01). STEADI Materials for Your Older Adult Patients. Retrieved March 15, 2016.
³CDC. (2016, March 14). Preventing Falls Among Older Adults. Retrieved March 15, 2016.
The Brain Injury Association of America (BIAA) has put together the following Fact Sheet with statistics and other information to raise awareness and educate the public about brain injuries.
Brain Injury Association of America (BIAA), T. (2015). Brain Injury Facts & Statistics. Retrieved February 29, 2016.
People who have had a moderate or severe head injury may spend weeks or months in hospital before they are ready to go on to rehabilitation or to return home. Whether you go straight home from hospital, or into a neuro-rehabilitation center, depends on your needs. Before you leave hospital, you will have an assessment and be given a care plan. This will outline the next steps to help your recovery, such as physiotherapy or speech therapy.
Once you are ready to go home, you may still need help in order to become more independent and reach your goals. You should continue to get therapy from a community-based team. It is worth finding out what services are available near you to get as much help as you can. For example, you may qualify for state benefits or you may be able to get adjustments to your home, special equipment, help with chores around the house, special transport, or advice on getting back to work.
Everyday activities
You may be impatient to get back to your everyday routine and resume activities like driving or going to work. However, it is important to give yourself time to adjust and recover. The time it takes will be different from person to person and what is enough time for one person may not be enough for another. For some people, it may not be realistic to go back to life as it was before the head injury.
Can I drive?
Having a serious head injury will most likely affect your right to hold a current driving licence. You are legally obliged to notify the Driver and Vehicle Licensing Agency (DVLA) about your condition and must not drive until you have DVLA approval. You might be permitted to resume driving once a doctor has confirmed that you have made a full recovery.
If you are experiencing problems as a result of the injury you might not be allowed to drive for a given period of time (often one year). The DVLA might give your General Practitioner (GP) this information instead of giving it directly to you. If you have seizures, this period might be extended until the seizures are controlled. If you continue driving without DVLA approval, insurers will not be obliged to meet any costs and you might be uninsured. This would make you personally liable for any damage you cause to others.
If you have any disabilities you will probably need a medical examination to be certain you can control a vehicle safely. Also, modifications to your vehicle might be required and your vision will also be checked. You can re-apply for your licence before the date you are scheduled to return to driving so that it is ready by the time this date comes around. However, you will probably only be given a three year licence. Furthermore, many insurance companies increase the rates for people who have had a head injury, so you might need to consider changing your insurance provider to get a more affordable policy. Regulations are stricter for HGV (Heavy Goods Vehicle) or PSV (Public Service Vehicle) licences.
Can I fly?
Yes, depending on your recovery. There is nothing to stop you from flying once you are fit enough to do so. You might experience headaches during take-off and landing due to pressure changes. You should increase your fluid intake, but try to avoid alcohol and caffeine as these can dehydrate the brain and increase the risk of headaches. Keep in mind that air travel can be stressful for people in good health so it can be especially stressful if you are feeling unwell.
Can I play sports?
Everyone is affected differently by head injuries and you will need to take it easy during your recovery. This means that it may not be appropriate for you to embark on an exercise regime for months after your injury. You will go through a period of rehabilitation with physiotherapy and occupational therapy exercises that will help you regain basic physical skills.
Your physiotherapist, GP, or specialist will tell you what type of physical activity is suitable for you and when you can start increasing your levels of activity. You should avoid all contact sports like rugby, boxing or martial arts, and strenuous exercise like lifting weights, for at least six months. You can then discuss with your specialist the possibility of resuming these sports if you wish to.
Can I drink alcohol?
You should not drink any alcohol for the first three weeks after sustaining a head injury. After that period of time, small amounts of alcohol are safe (although you are likely to feel the effects more than you used to). There is also a risk of provoking a seizure if you drink too much. Some people find that they have more severe hangovers after a head injury. If you are taking any medication – especially anti-epileptic drugs – you should check with your doctor if it is safe to drink alcohol.
When can I go back to work?
After your head injury you may not be able to do all the things you previously could. You may be affected by psychological problems, like memory and concentration, and physical problems, such as mobility. It is important to take things slowly, like not returning to work before you are ready, and consider ways in which you could adapt your work or workplace to make things easier for you.
Before returning to work, you should check with your GP or specialist to make sure they agree you are ready. If appropriate, many people find it helpful to go back part-time or for a few hours each week before returning to full-time status. Neurosupport, the charity providing non-medical information and support to people with neurological conditions, runs an Employment and Community Service to help and advise people affected by brain injuries with any issues to do with employment or in finding a meaningful alternative to work. When someone has had a serious head injury, it is hard to know what will happen in the future, how the person will recover and what kind of care they will need.
Want more information?
Visit the Brain Injury Association of America or the Brain Injury Association of Michigan to learn more about living with a brain injury.
For information on home care options for you or a loved one, visit Our Specialties page or give us a call at 866-8668984!
Brain & Spine Foundation (2013, October) Going home and rehabilitation after a moderate to severe head injury. Retrieved February, 26, 2016.
A Traumatic Brain Injury (TBI) refers to the amount of damage done to the brain tissue resulting from a closed or open head injury. The Glasgow Coma Scale (GCS) is most often used by doctors to determine the category of the TBI in which the “severity” ranges from mild (briefly disoriented/loss of consciousness) to moderate to severe (unconscious for an extended period of time).
No two brain injuries are the same. However, because this injury affects the brain, major lifestyle (and possibly personality) changes might occur. For example, you or someone you know who suffered a TBI may now require either short-term or long-term care. In the following article, we will list the initial aspects of a Traumatic Brain Injury.
What causes a TBI?
A blow to the head can occur from a variety of accidents. Some examples include:
- A motor vehicle crash
- Sports injuries
- A fall
- Assaults
- A bicycle crash
- Military service-related injuries
- Child abuse/domestic violence incidents
- The skull being struck by a blunt or heavy object
Common Symptoms After a Mild TBI
- Headaches
- Bruises—When the head is hit, the brain can be shaken around inside the skull. If the shaking was hard enough, the brain can get bruised as it hits the skull. Just like bruises you might get on your arms or legs, these go away in time.
- Swelling— If there are lots of bruises, there also might be swelling. Swelling takes longer than bruising to return to normal.
- Dizziness
- Nausea and sensitivity to light and sound
- Snapped nerve fibers—The brain is made of millions of cells called neurons that are connected to each other by long, thin fibers called axons. If the TBI is serious enough, some of these axons can snap or break during a concussion. When this happens, different cells in your brain cannot communicate properly with each other. With time, however, these will heal and many patients have a complete recovery.
- Broken blood vessels—Like any other part of the body, the brain has blood vessels in it. If a TBI is very serious, some of these blood vessels can tear and bleed soon after the injury. Usually, the bleeding stops on its own and the blood vessels heal like any other cut does.
It’s important to note that these symptoms may not occur right away and could appear days or even weeks after the accident.
Determining the level of the TBI
- Severity of initial injury
- Rate/completeness of physiological recovery
- Functions affected such as cognitive, motor, sensory, verbal, and emotion
- Meaning of dysfunction in the individual’s life
- Resources available to aid recovery of function
Where can you go for support?
- Brain Injury Association of Michigan (BIAMI) Helpline: 800-772-4323 or www.biami.org.
- Michigan Department of Community Health TBI website, www.michigan.gov/tbi, has many free educational materials including:
- Michigan Resource Guide for Persons with Traumatic Brain Injury and Their Families, a 96-page directory of resources that provides information about TBI, the signs of TBI and a wide variety of services that are available.
- Dobson Healthcare: 866-866-8984 or www.dobsonhealthcare.com.
Evans, R.W., Evans, R.I., & Sharp, M.J. (1994). The physician survey on the post-concussion and whiplash syndromes. Headache, 34, 268-74.
Kashluba, S., Paniak, C., Blake, T., et al. (2004). A longitudinal, controlled study of patient complaints following treated mild traumatic brain injury.
Archives of Clinical Neuropsychology. 19, 805-816.
McCrea, M., Guskiewicz, K.M., Marshall, S.W., et al. (2003). Acute Effects and Recovery Time Following Concussion in Collegiate Football
Players – The NCAA Concussion Study. Journal of the American Medical Association, 290, 2556-2563.
Mittenberg, W., Zielinski, R.E., & Fichera, S. (1993). Recovery from mild head injury: A treatment manual for Patients. Psychotherapy in Private
Practice, 12, 37-52.
Mount Sinai Medical Center. (n.d.). What Happens Immediately After the Injury? Retrieved February 10, 2016 from brainline.org.
Rohling, M.L., Meyers, J.E., & Millis, S.R. (2003). Neuropsychological Impairment Following Traumatic Brain Injury: A Dose-Response Analysis.
The Clinical Neurolopsycholoigist 17, 289-302.
Traumatic Brain Injury.com, LLC. (n.d.). Mild TBI Symptoms. Retrieved February 10, 2016, from traumaticbraininjury.com.
Traumatic Brain Injury.com, LLC. (n.d.). Severe TBI Symptoms. Retrieved February 10, 2016, from traumaticbraininjury.com.
Photo: Chlossser, M. (2015). Slip and Fall Accidents the Leading Cause of Traumatic Brain Injury. Retrieved February 10, 2016.
Incidence of brain injury
• 1.7 million people sustain a traumatic brain injury (TBI) each year. According to the Centers for Disease Control and Injury Prevention, the leading causes of TBI are:
o Falls (35.2%)
o Motor vehicle-traffic crashes (17.3%)
o Struck by/against events (16.5%)
o Assaults (10%)
• Brain injury can result in a range of outcomes (according to the Centers for Disease Control and Prevention):
o 52,000 die
o 275,000 are hospitalized
o 1,365,000 are treated and released from an emergency department.
• According to the Centers for Disease Control and Prevention, among children ages 0 to 14 years, TBI results in an estimated
o 2,685 deaths
o 37,000 hospitalizations
o 435,000 emergency department visits
• The number of people with TBI who are not seen in an emergency department or who receive no care is unknown.
• TBI is a contributing factor to a third (30.5%) of all injury-related deaths in the United States.
5
• About 75% of TBIs that occur each year are concussions or other forms of mild traumatic brain injury (MTBI).
Source: Brain Injury Association of America
Children who sustain a traumatic brain injury at a younger age have different results as they heal than those who are older. At Dobson we are able to provide services to children as they recover at home from a traumatic brain injury. Our specially trained staff for Certified Brain Injury Specialists can assist with all levels of care during the recovering process.
Check out this article from cnn.com for more information.
Severe Traumatic Brain Injury Affects Development in Young Children