According to the Centers for Disease Control & Prevention,
“…more than 60,000 young children end up in emergency rooms every year because they get into medicines when their parent or caregiver isn’t looking…” (CDC, 2011).
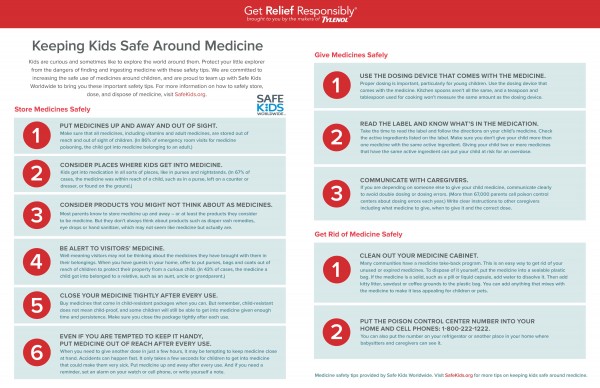
This statistics resonates with us because our some of our caregivers take care of clients who have children in their homes. With medication assistance part of our Person Care Services, we felt it was important to share medication safety precautions during National Patient Safety Awareness Week. Please read through the safety guidelines from Safe Kids World Wide to help increase the safe use of medications around children.
CDC. (2011). Put Your Medicines Up and Away and Out of Sight. Retrieved March 14, 2016.
Safe Kids Worldwide, & Tylenol. (n.d.). Keeping Kids Safe Around Medicine. Retrieved March 14, 2016.
Our home healthcare caregivers work directly with individuals within the comfort of our client’s own home. Because of this, Dobson Healthcare and our caregivers have little control over the work environment, which may contain a number of safety and health hazards. In their overview of home healthcare hazards, OSHA states “…these hazards [could] include bloodborne pathogens and biological hazards, latex sensitivity, ergonomic hazards from patient lifting, violence, hostile animals and unhygienic and dangerous conditions…” (United States Department of Labor).
Safety is a top priority for our caregivers and our clients. We want to ensure we are sending our caregivers into a home that will not pose a threat that person’s health. We must also ensure our client’s safety by taking actions such as simply changing the batteries in a smoke detector or reporting dangerous conditions to the proper authorities. Dobson Healthcare and the National Patient Safety Foundation recognizes the week of March 13-19, 2016 and National Patient Safety Awareness Week. To begin our week, we wanted to share some Basic Safety Rules to help increase awareness about patient safety.
Community Health Network. (n.d.). Home safety tips. Retrieved March 11, 2016.
United States Department of Labor. (n.d.). Home Healthcare. Retrieved March 11, 2016.
As stated by The World Kidney Team “…The importance of identifying and treating childhood kidney diseases, instilling an awareness of the risks for their future from kidney damage that originates in childhood, therefore building healthier future generations!” The more you learn about Kidney Disease, the better your chances are for preventing it. Learn more about the campaign at www.worldkidneyday.org.
What can you do for your kidneys?
Kidney diseases are silent killers, which will largely affect your quality of life. There are however several easy ways to reduce the risk of developing kidney disease.
Keep fit and active
Keeping fit helps to reduce your blood pressure and therefore reduces the risk of Chronic Kidney Disease.
The concept “on the move for kidney health” is a worldwide collective march involving the public, celebrities and professionals moving across a public area by walking, running and cycling. Why not join them – by whatever means you prefer! Check out the events section of the WKD website for more information.
Keep regular control of your blood sugar level
About half of people who have diabetes develop kidney damage, so it is important for people with diabetes to have regular tests to check their kidney functions.
Kidney damage from diabetes can be reduced or prevented if detected early. It is important to keep control of blood sugar levels with the help of doctors or pharmacists, who are always happy to help.
Monitor your blood pressure
Although many people may be aware that high blood pressure can lead to a stroke or heart attack, few know that it is also the most common cause of kidney damage.
The normal blood pressure level is 120/80. Between this level and 139/89, you are considered prehypertensive and should adopt lifestyle and dietary changes. At 140/90 and above, you should discuss the risks with your doctor and montior your blood pressure level regularly. High blood pressure is especially likely to cause kidney damage when associated with other factors like diabetes, high cholesterol and Cardio- Vascular Diseases.
Eat healthy and keep your weight in check
This can help prevent diabetes, heart disease and other conditions associated with Chronic Kidney Disease.
Reduce your salt intake. The recommended sodium intake is 5-6 grams of salt per day (around a teaspoon). In order to reduce your salt intake, try and limit the amount of processed and restaurant food and do not add salt to food. It will be easier to control your intake if you prepare the food yourself with fresh ingredients. For more information on nutrition and kidney friendly cooking, visit our nutrition page
Maintain a healthy fluid intake
Although clinical studies have not reached an agreement on the ideal quantity of water and other fluids we should consume daily to maintain good health, traditional wisdom has long suggested drinking 1.5 to 2 litres (3 to 4 pints) of water per day.
Consuming plenty of fluid helps the kidneys clear sodium, urea and toxins from the body which, in turn, results in a “significantly lower risk” of developing chronic kidney disease, according to researchers in Australia and Canada. The findings, the researchers said, do not advocate “aggressive fluid loading”, which can cause side effects, but they do provide evidence that moderately increased water intake, around two litres daily, may reduce the risk of decline in kidney function. It’s important to keep in mind that the right level of fluid intake for any individual depends on many factors including gender, exercise, climate, health conditions, pregnancy and breast feeding. In addition, people who have already had a kidney stone are advised to drink 2 to 3 litres of water daily to lessen the risk of forming a new stone.
Do not smoke
Smoking slows the flow of blood to the kidneys. When less blood reaches the kidneys, it impairs their ability to function properly. Smoking also increases the risk of kidney cancer by about 50 percent.
Do not take over-the-counter pills on a regular basis
Common drugs such non-steroidal anti-inflammatory drugs like ibuprofen are known to cause kidney damage and disease if taken regularly.
Such medications probably do not pose significant danger if your kidneys are relatively healthy and you use them for emergencies only, but if you are dealing with chronic pain, such as arthritis or back pain, work with your doctor to find a way to control your pain without putting your kidneys at risk.
World Kidney Day. (2013, August 28). 8 Golden Rules. Retrieved March 10, 2016.
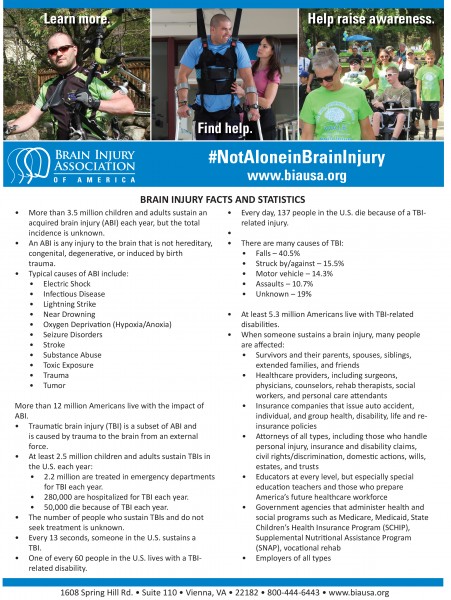
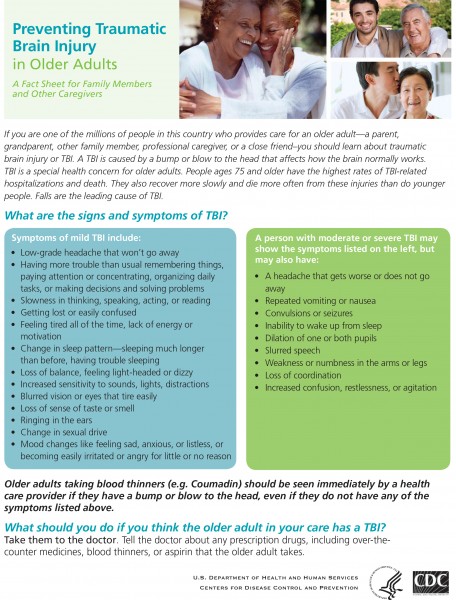
The Brain Injury Association of America (BIAA) has put together the following Fact Sheet with statistics and other information to raise awareness and educate the public about brain injuries.
Brain Injury Association of America (BIAA), T. (2015). Brain Injury Facts & Statistics. Retrieved February 29, 2016.
People who have had a moderate or severe head injury may spend weeks or months in hospital before they are ready to go on to rehabilitation or to return home. Whether you go straight home from hospital, or into a neuro-rehabilitation center, depends on your needs. Before you leave hospital, you will have an assessment and be given a care plan. This will outline the next steps to help your recovery, such as physiotherapy or speech therapy.
Once you are ready to go home, you may still need help in order to become more independent and reach your goals. You should continue to get therapy from a community-based team. It is worth finding out what services are available near you to get as much help as you can. For example, you may qualify for state benefits or you may be able to get adjustments to your home, special equipment, help with chores around the house, special transport, or advice on getting back to work.
Everyday activities
You may be impatient to get back to your everyday routine and resume activities like driving or going to work. However, it is important to give yourself time to adjust and recover. The time it takes will be different from person to person and what is enough time for one person may not be enough for another. For some people, it may not be realistic to go back to life as it was before the head injury.
Can I drive?
Having a serious head injury will most likely affect your right to hold a current driving licence. You are legally obliged to notify the Driver and Vehicle Licensing Agency (DVLA) about your condition and must not drive until you have DVLA approval. You might be permitted to resume driving once a doctor has confirmed that you have made a full recovery.
If you are experiencing problems as a result of the injury you might not be allowed to drive for a given period of time (often one year). The DVLA might give your General Practitioner (GP) this information instead of giving it directly to you. If you have seizures, this period might be extended until the seizures are controlled. If you continue driving without DVLA approval, insurers will not be obliged to meet any costs and you might be uninsured. This would make you personally liable for any damage you cause to others.
If you have any disabilities you will probably need a medical examination to be certain you can control a vehicle safely. Also, modifications to your vehicle might be required and your vision will also be checked. You can re-apply for your licence before the date you are scheduled to return to driving so that it is ready by the time this date comes around. However, you will probably only be given a three year licence. Furthermore, many insurance companies increase the rates for people who have had a head injury, so you might need to consider changing your insurance provider to get a more affordable policy. Regulations are stricter for HGV (Heavy Goods Vehicle) or PSV (Public Service Vehicle) licences.
Can I fly?
Yes, depending on your recovery. There is nothing to stop you from flying once you are fit enough to do so. You might experience headaches during take-off and landing due to pressure changes. You should increase your fluid intake, but try to avoid alcohol and caffeine as these can dehydrate the brain and increase the risk of headaches. Keep in mind that air travel can be stressful for people in good health so it can be especially stressful if you are feeling unwell.
Can I play sports?
Everyone is affected differently by head injuries and you will need to take it easy during your recovery. This means that it may not be appropriate for you to embark on an exercise regime for months after your injury. You will go through a period of rehabilitation with physiotherapy and occupational therapy exercises that will help you regain basic physical skills.
Your physiotherapist, GP, or specialist will tell you what type of physical activity is suitable for you and when you can start increasing your levels of activity. You should avoid all contact sports like rugby, boxing or martial arts, and strenuous exercise like lifting weights, for at least six months. You can then discuss with your specialist the possibility of resuming these sports if you wish to.
Can I drink alcohol?
You should not drink any alcohol for the first three weeks after sustaining a head injury. After that period of time, small amounts of alcohol are safe (although you are likely to feel the effects more than you used to). There is also a risk of provoking a seizure if you drink too much. Some people find that they have more severe hangovers after a head injury. If you are taking any medication – especially anti-epileptic drugs – you should check with your doctor if it is safe to drink alcohol.
When can I go back to work?
After your head injury you may not be able to do all the things you previously could. You may be affected by psychological problems, like memory and concentration, and physical problems, such as mobility. It is important to take things slowly, like not returning to work before you are ready, and consider ways in which you could adapt your work or workplace to make things easier for you.
Before returning to work, you should check with your GP or specialist to make sure they agree you are ready. If appropriate, many people find it helpful to go back part-time or for a few hours each week before returning to full-time status. Neurosupport, the charity providing non-medical information and support to people with neurological conditions, runs an Employment and Community Service to help and advise people affected by brain injuries with any issues to do with employment or in finding a meaningful alternative to work. When someone has had a serious head injury, it is hard to know what will happen in the future, how the person will recover and what kind of care they will need.
Want more information?
Visit the Brain Injury Association of America or the Brain Injury Association of Michigan to learn more about living with a brain injury.
For information on home care options for you or a loved one, visit Our Specialties page or give us a call at 866-8668984!
Brain & Spine Foundation (2013, October) Going home and rehabilitation after a moderate to severe head injury. Retrieved February, 26, 2016.
If you or a loved one has been diagnosed with a cardiovascular disease, you may require Infusion Therapy in order to receive your medicine. Infusion Therapy involves administering nutrition and medication intravenously, or directly into the veins, through the use of a needle or catheter. Many Infusion Therapy candidates require treatment for heart diseases such as congestive heart failure and coronary heart disease. For those needing long-term therapy, the more popular and more comfortable setting choice is home infusion rather than an inpatient setting.
We at Dobson, specialize in providing skilled, infusion nurses who are knowledgeable in the care and monitoring a variety of infusion therapies. These skilled professionals can assist the patient and family in the coordination and management of your infusion patient’s care. Infusion nurses are able to provide a personalized, professional care to each patient in order to meet the needs of their specific therapy. To learn more about our Infusion Services, read our Fact Sheet below or give us a call at 866-866-8984!
National Home Infusion Association. (n.d.). Infusion FAQs. Retrieved February 22, 2016
According to the National Heart, Lung, and Blood Institute, a diagnosis of a cardiovascular disease is “…based on your medical and family histories, your risk factors, a physical exam, and the results from tests and procedures” (National Heart, Lung, and Blood Institute, 2014). Below you will find a brief explanation of a few of these screening tests. If you feel you are at risk for heart disease, we encourage you to talk to your doctor about these tests, his or her recommendation for you, and what the results of the test(s) will mean.
American Heart Association. (2014, October 21). Heart-Health Screenings. Retrieved February 18, 2016.
American Heart Association. (2015). What is a Stress Test? Retrieved February 18, 2016.
National Heart, Lung, and Blood Institute. (2012, February 29). The Heart Truth® for Women: If You Have Heart Disease. Retrieved February 18, 2016.
National Heart, Lung, and Blood Institute. (2014, April 21). How Is Heart Disease Diagnosed? Retrieved February 18, 2016.
National Heart, Lung, and Blood Institute. (2011, October 31). What Does Echocardiography Show? Retrieved February 18, 2016.
WebMD. (2014, August 13). Heart Tests: When Do You Need Them? Retrieved February 18, 2016.
WebMD. (2014, September 26). What Is an Electrocardiogram (EKG or ECG) Test? Retrieved February 18, 2016.
Photo: Blood Clotting Nemesis of Life. (n.d.). Retrieved February 18, 2016.
Photo: Gwinnett Clinic. (n.d.). Cardiac Testing. Retrieved February 18, 2016.
Photo: Echocardiographer.org. (n.d.). Transthoracic Echo. Retrieved February 18, 2016.
Photo: ECG Wave-Maven. (2015, June 6). Diagnostic Cardiac Catheterization and Coronary Angiography. Retrieved February 18, 2016
A Traumatic Brain Injury (TBI) refers to the amount of damage done to the brain tissue resulting from a closed or open head injury. The Glasgow Coma Scale (GCS) is most often used by doctors to determine the category of the TBI in which the “severity” ranges from mild (briefly disoriented/loss of consciousness) to moderate to severe (unconscious for an extended period of time).
No two brain injuries are the same. However, because this injury affects the brain, major lifestyle (and possibly personality) changes might occur. For example, you or someone you know who suffered a TBI may now require either short-term or long-term care. In the following article, we will list the initial aspects of a Traumatic Brain Injury.
What causes a TBI?
A blow to the head can occur from a variety of accidents. Some examples include:
- A motor vehicle crash
- Sports injuries
- A fall
- Assaults
- A bicycle crash
- Military service-related injuries
- Child abuse/domestic violence incidents
- The skull being struck by a blunt or heavy object
Common Symptoms After a Mild TBI
- Headaches
- Bruises—When the head is hit, the brain can be shaken around inside the skull. If the shaking was hard enough, the brain can get bruised as it hits the skull. Just like bruises you might get on your arms or legs, these go away in time.
- Swelling— If there are lots of bruises, there also might be swelling. Swelling takes longer than bruising to return to normal.
- Dizziness
- Nausea and sensitivity to light and sound
- Snapped nerve fibers—The brain is made of millions of cells called neurons that are connected to each other by long, thin fibers called axons. If the TBI is serious enough, some of these axons can snap or break during a concussion. When this happens, different cells in your brain cannot communicate properly with each other. With time, however, these will heal and many patients have a complete recovery.
- Broken blood vessels—Like any other part of the body, the brain has blood vessels in it. If a TBI is very serious, some of these blood vessels can tear and bleed soon after the injury. Usually, the bleeding stops on its own and the blood vessels heal like any other cut does.
It’s important to note that these symptoms may not occur right away and could appear days or even weeks after the accident.
Determining the level of the TBI
- Severity of initial injury
- Rate/completeness of physiological recovery
- Functions affected such as cognitive, motor, sensory, verbal, and emotion
- Meaning of dysfunction in the individual’s life
- Resources available to aid recovery of function
Where can you go for support?
- Brain Injury Association of Michigan (BIAMI) Helpline: 800-772-4323 or www.biami.org.
- Michigan Department of Community Health TBI website, www.michigan.gov/tbi, has many free educational materials including:
- Michigan Resource Guide for Persons with Traumatic Brain Injury and Their Families, a 96-page directory of resources that provides information about TBI, the signs of TBI and a wide variety of services that are available.
- Dobson Healthcare: 866-866-8984 or www.dobsonhealthcare.com.
Evans, R.W., Evans, R.I., & Sharp, M.J. (1994). The physician survey on the post-concussion and whiplash syndromes. Headache, 34, 268-74.
Kashluba, S., Paniak, C., Blake, T., et al. (2004). A longitudinal, controlled study of patient complaints following treated mild traumatic brain injury.
Archives of Clinical Neuropsychology. 19, 805-816.
McCrea, M., Guskiewicz, K.M., Marshall, S.W., et al. (2003). Acute Effects and Recovery Time Following Concussion in Collegiate Football
Players – The NCAA Concussion Study. Journal of the American Medical Association, 290, 2556-2563.
Mittenberg, W., Zielinski, R.E., & Fichera, S. (1993). Recovery from mild head injury: A treatment manual for Patients. Psychotherapy in Private
Practice, 12, 37-52.
Mount Sinai Medical Center. (n.d.). What Happens Immediately After the Injury? Retrieved February 10, 2016 from brainline.org.
Rohling, M.L., Meyers, J.E., & Millis, S.R. (2003). Neuropsychological Impairment Following Traumatic Brain Injury: A Dose-Response Analysis.
The Clinical Neurolopsycholoigist 17, 289-302.
Traumatic Brain Injury.com, LLC. (n.d.). Mild TBI Symptoms. Retrieved February 10, 2016, from traumaticbraininjury.com.
Traumatic Brain Injury.com, LLC. (n.d.). Severe TBI Symptoms. Retrieved February 10, 2016, from traumaticbraininjury.com.
Photo: Chlossser, M. (2015). Slip and Fall Accidents the Leading Cause of Traumatic Brain Injury. Retrieved February 10, 2016.