An estimated 12,500 spinal cord injuries occur in the U.S. every year, leaving the injured people, their friends, and their family, to cope with the aftermath of the catastrophe. For many, navigating the challenges of the health care system can feel a bit like going to medical school. Suddenly you’re learning a veritable cornucopia of new terms, and may be spending endless hours Googling spinal cord anatomy to fill in the gaps in your knowledge.
An educated patient is better equipped to advocate for his or her needs and interests. An education in spinal cord anatomy helps you understand what your doctor is saying, ask intelligent questions, and detect medical errors before they endanger your health.
Spinal Cord Anatomy: The Basics
Though you might think of your spinal cord as one single piece, it’s actually a column of nerves protected by a sheath of myelin and then further secured by 31 butterfly-shaped vertebrae (singular: vertebra).
Medical providers divide the spinal cord into four distinct regions. Knowing the region in which the injury is located is often the key to understanding diagnosis and treatment. The four spinal cord regions are:
- The cervical spinal cord: This is the topmost portion of the spinal cord, where the brain connects to the spinal cord, and the neck connects to the back. This region consists of eight vertebrae, commonly referred to as C1-C8. All spinal cord numbers are descending, so C1 is the highest vertebra, while C8 is the lowest in this region.
- The thoracic spinal cord: This section forms the middle of the spinal cord, containing twelve vertebrae numbered T1-T12.
- The lumbar spinal cord: This is a lower region of the spinal cord, where your spinal cord begins to bend. If you put your hand in your lower back, where your back bends inward, you’re feeling your lumbar region. There are five lumbar vertebrae, numbered L1-L5.
- The sacral spine: This is the lower, triangle-shaped region of the spine, also with five vertebrae. While the lumbar cord bends inward, the vertebrae of the sacral region bend slightly outward. There is no actual spinal cord in this section, it is made up of nerve roots which exit the spine at their respective vertebral levels.
- The coccygeal region, sometimes known as the coccyx or tail bone, consists of a single vertebra at the very base of the spinal cord.
Types of Spinal Cord Injuries
All spinal cord injuries are divided into two broad categories: incomplete and complete.
- Incomplete spinal cord injuries: With incomplete injuries, the cord is only partially severed, allowing the injured person to retain some function. In these cases, the degree of function depends on the extent of the injuries.
- Complete spinal cord injuries: By contrast, complete injuries occur when the spinal cord is fully severed, eliminating function. Though, with treatment and physical therapy, it may be possible to regain some function.
Incomplete spinal cord injuries are increasingly common, thanks in part to better treatment and increased knowledge about how to respond—and how not to respond—to a suspected spinal cord injury. These injuries now account for more than 60% of spinal cord injuries, which means we’re making real progress toward better treatment and better outcomes.
Some of the most common types of incomplete or partial spinal cord injuries include:
- Anterior cord syndrome: This type of injury, to the front of the spinal cord, damages the motor and sensory pathways in the spinal cord. You may retain some sensation, but struggle with movement.
- Central cord syndrome: This injury is an injury to the center of the cord, and damages nerves that carry signals from the brain to the spinal cord. Loss of fine motor skills, paralysis of the arms, and partial impairment—usually less pronounced—in the legs are common. Some survivors also suffer a loss of bowel or bladder control, or lose the ability to sexually function.
- Brown-Sequard syndrome: This variety of injury is the product of damage to one side of the spinal cord. The injury may be more pronounced on one side of the body; for instance, movement may be impossible on the right side, but may be fully retained on the left. The degree to which Brown-Sequard patients are injured greatly varies from patient to patient.
Knowing the location of your injury and whether or not the injury is complete can help you begin researching your prognosis and asking your doctor intelligent questions. Doctors assign different labels to spinal cord injuries depending upon the nature of those injuries. The most common types of spinal cord injuries include:
- Tetraplegia: These injuries, which are the result of damage to the cervical spinal cord, are typically the most severe, producing varying degrees of paralysis of all limbs. Sometimes known as quadriplegia, tetraplegia eliminates your ability to move below the site of the injury, and may produce difficulties with bladder and bowel control, respiration, and other routine functions. The higher up on the cervical spinal cord the injury is, the more severe symptoms will likely be.
- Paraplegia: This occurs when sensation and movement are removed from the lower half of the body, including the legs. These injuries are the product of damage to the thoracic spinal cord. As with cervical spinal cord injuries, injuries are typically more severe when they are closer to the top vertebra.
- Triplegia: Triplegia causes loss of sensation and movement in one arm and both legs, and is typically the product of an incomplete spinal cord injury.
Injuries below the lumbar spinal cord do not typically produce symptoms of paralysis or loss of sensation. They can, however, produce nerve pain, reduce function in some areas of the body, and necessitate several surgeries to regain function. Injuries to the sacral spinal cord, for instance, can interfere with bowel and bladder function, cause sexual problems, and produce weakness in the hips or legs. In vary rare cases, sacral spinal cord injury survivors suffer temporary or partial paralysis.
SOURCE: SpinalCord.Com

Children who sustain a traumatic brain injury at a younger age have different results as they heal than those who are older. At Dobson we are able to provide services to children as they recover at home from a traumatic brain injury. Our specially trained staff for Certified Brain Injury Specialists can assist with all levels of care during the recovering process.
Check out this article from cnn.com for more information.
Severe Traumatic Brain Injury Affects Development in Young Children
“YOU NEED TO FIND A CASE MANAGER”, says the nurse, social worker or discharge planner. As reality begins to “hit you between the eyes” following the brain injury of a loved one, many terms will be “thrown at you” and often you, the survivor are so overwhelmed that even the decision of when to take your next breath, seems difficult. For the next few months, I will attempt to assist you in understanding some of various words and phrases you will hear through this sometimes difficult journey.
Let’s start with the term CASE MANAGER:
A case manager is a health care professional, typically a nurse, rehab counselor or a social worker whose job is to manage your loved ones health care services and advocate (be the voice of) their client, your loved one. Their goals for their clients include but are not limited to:
1. Help their clients enjoy the highest quality of life possible
2. Maximize the use of available benefits, resources and services
3. Assist them to live as independently as possible and smoothly help to integrate them back into the community when able
Case managers do these things to assist their clients to recover to the best of their ability. It is the case manager’s responsibility to achieve these goals in a cost-effective way assuring the health and safety of your loved one. In short, you and your case manager have the same goals. A good case manager has the knowledge, skills and experience to accomplish these goals. Case management typically should start within weeks of the injury but, it can begin and end at any time throughout the lifelong recovery process.
The big question for all survivors is Where do I find one? How do I find one? Contact your state brain injury association or the Brain Injury Association of America for names of local case managers, check your yellow pages under rehabilitation, google “case managers” in (your town/state), ask health care professionals, pharmacists, your insurance company, etc. When your loved one is in the hospital, an inpatient rehab facility or day rehab program, there will be an “in-house” case manager/social worker who will do your “negotiating” for you. Your health insurance company may provide a case manager to oversee reimbursable medical services but long term, after discharge you may still need a case management advocate on your team.
REMEMBER…YOU ARE THE BOSS! A case manager can and should be interviewed by you just like any member of your loved one’s “team”.
You or your loved one will then become their “employer”. Some things to consider when interviewing a case manager are:
1. Is he/she licensed in her profession?
2. Is he/she a certified brain injury specialist? (CBIS) (not mandatory but very helpful)
3. How long has he/she been representing brain injured victims?
4. How many families has he/she helped?
5. ASK FOR REFERENCES
6. Does he/she sound informed about brain injury?
7. Does he/she seem to understand the issues you are facing?
8. What are the costs?
9. Will you and your loved one feel comfortable working with this person for weeks, months and, possibly, years?
10. How frequently will he/she communicate with you and how? In person, phone, email, and/or fax?
Keep in mind that your case manager works for your loved one. You have the right to “fire” them if you do not feel they are working in your loved ones best interest.
As a side note, look for a support group for TBI families and victims. Ask ICU/CCU nurses, physicians, friends to put you in touch with other families who are experiencing or have experienced the same “journey” you and your loved one are traveling right now. They will be thrilled to help. Again, we can only keep what we have by giving it away and especially for TBI survivors and their families, as they all wish they had the knowledge that only comes from going through the very unfortunate experience that they have.
Source: Successfully Surviving a Brain Injury-A Family Guidebook by Garry Prowe
First things first…Important to remember…
- A person with a brain injury is a person first
- No two brain injuries are exactly the same
- The effects of any brain injury are complex and vary greatly with each person
- The effects of any brain injury depend on things like cause, location of the brain injury and severity of the injury
Let’s talk about the “lobes” or sections of the brain. There are four: Frontal, Temporal, Parietal and Occipital. This will be very basic information about each of the lobes of the brain. Some behaviors/deficits may be explained by knowing which section of the brain is injured, and by understanding the basic functions of those lobes.
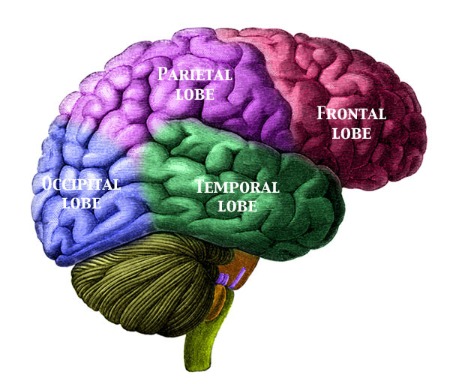
Frontal Lobe: Situated at the front of the skull, the “forehead region”, our frontal lobes are known as our emotional control center and are also, “home to our personality”. The frontal lobe is associated with motor skills, reasoning, higher level awareness/cognition and expressive language. This lobe receives information from other lobes of the brain and utilizes it to carry out body movements.
Temporal Lobes: Located on either side of the skull, above the ear, the temporal lobes are associated with visual and auditory (hearing) input. They provide the organization of the input. Persons with injury to the temporal lobe may have difficulty placing words or pictures into categories. They are highly associated with memory skills. Left temporal injury may result in impaired memory for verbal material, while right temporal injury may result in the inability to recall non verbal material, i.e. music, drawings. Severe damage to the temporal lobe may also increase unfavorable sexual behavior.
Parietal Lobe: The parietal lobe is the middle section of the brain, located near the back and top of the head. This lobe is responsible for processing tactile sensory information such as touch, pain, pressure, etc. An important section of the brain is located in the parietal lobe and is essential to the processing of the body’s senses.
Occipital Lobe: The occipital lobe is located in the back portion of the brain. It is associated with vision. An important section of this lobe of the brain is the primary visual cortex. This area receives and interprets information from the retinas of the eyes. Damage to this lobe can cause a variety of visual disturbances and even blindness.
Again, no two brain injuries are exactly alike. Every person will respond and recover at a different rate. This is just meant to help you to understand a little more on why the deficit you may be seeing with your brain injured loved one, is present.
Hi!
My name is Darling Warner and I am an LPN and a Certified Brain Injury Specialist. Nearly 10 years ago, I took a leap of faith and changed my “comfort zone” nursing career from a quiet, stable office nurse and took on a very challenging new career in nursing taking care of Traumatic Brain Injury victims. I have not had one nano-second of regret since making that move and as a result, TBI has become my passion with regard to my nursing career.
I would like to share with you a “TBI TIDBIT” monthly. I’ll try to keep it simple and yet informative. If ever you have a question or if you are a TBI survivor or family member that just needs someone to talk to, I’m a phone call away. I look forward to hearing from you about different topics you would like for me to cover. Sharing my passion for TBI care with you is the greatest gift I could give!
Let’s start with the definition of a Traumatic Brain Injury:
Also referred to as a TBI, it is an injury to the brain in which an external event or object, i.e. auto, motorcycle or snowmobile accident, gunshot wound, a fall or an assault, is the cause. The “blow” to the head causes the brain to “collide” with the inside of the skull, which is immovable, causing a disruption in the “electricity” that is transferred from the brain to the rest of the body. The injury can vary from mild, to moderate or severe, and the recovery of the patient varies based on the severity of the injury.
Please look for my next post coming Mid-December that will discuss in detail the different degrees of a Traumatic Brain Injury.
Darling Warner can be contacted at darlingwarner@dobsonhealthcare.com or by calling (866) 866-8984
